The Multidimensional Maze of Emotional Barriers
We often mistake "emotional barriers" as mere romantic tribulations, yet life's true crucible extends far beyond lovers' quarrels. The real test manifests when we confront the invisible chains of parental expectations that shape our career choices, the suffocating weight of friendships demanding perpetual validation, or the obsessive grip of professional ambitions that eclipse life's simple joys. These are the seven-layer emotional labyrinbbath where most souls lose their way.
Modern neuroscience reveals an intriguing paradox: The brain registers emotional pain from social rejection in the anterior cingulate cortex - the same region that processes physical injury. This explains why unrequited familial love can feel like phantom limb pain, and professional failures might induce actual chest tightness.
Case Study:
Li Wei, 34, Shanghai finance executive
"Working 100-hour weeks to prove myself to disapproving parents nearly destroyed my marriage. The breakthrough came when I realized my workaholism wasn't about filial duty, but my own fear of mediocrity."
The Metamorphosis of Self-Awareness
True emotional transcendence begins with recognizing the mirror principle of human connections:
- Others' behavior towards us = Reflections of our past karma
- Our treatment of others = Current spiritual cultivation
This paradigm shift transforms victims into alchemists. As Buddhist teacher Thich Nhat Hanh observed: "When you understand the roots of others' suffering, your anger becomes compost for compassion."
Three Stages of Emotional Alchemy:

-
Obsessive Attachment
(Demanding reciprocal love like emotional bookkeeping)
-
Conscious Detachment
(The "I Release" epiphany captured in Taoist water imagery)
-
Enlightened Reengagement
(Loving freely without transactional expectations)
Adlerian Philosophy: The Courage to Be Disliked
Alfred Adler's revolutionary concept of "Gemeinschaftsgefühl" (community feeling) paradoxically advocates:
- Complete self-acceptance → Authentic social harmony
- Indifference to external validation → Genuine interpersonal connections
Corporate Warrior's Epiphany:
James, 42, New York hedge fund manager
"Chasing promotions to impress college rivals left me empty. Now leading a fintech startup, I sleep soundly even when VCs question my 'unambitious' growth targets."
The Hardware-Software Matrix of Emotional Autonomy

| Hardware Independence 🖥️ |
Software Resilience 🧠 |
| • Economic self-sufficiency |
• Non-attachment to outcomes |
| • Transferable expertise |
• Self-validating mindset |
| • Needs < Income |
• Curiosity-driven purpose |
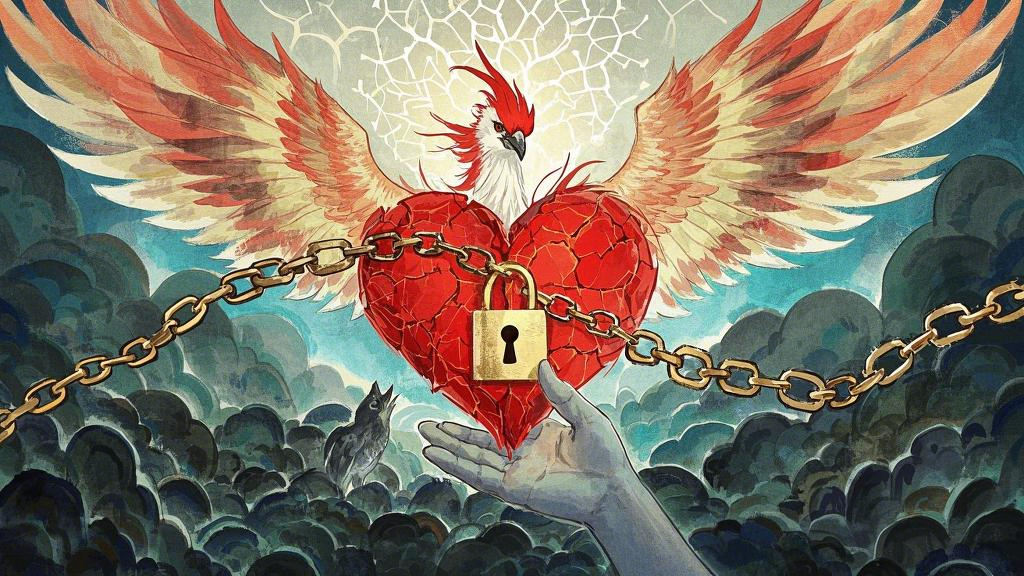
The Phoenix Curriculum: Forging Unshakable Inner Strength

1. Shadow Work Rituals
- Weekly "emotional archaeology" journaling
- Identifying recurring relationship patterns as spiritual breadcrumbs
2. Karma Yoga in Action
- Volunteering without resume-building motives
- Practicing "stealth kindness" (anonymous good deeds)
3. Cognitive Firewalking
- Intentionally reading critical reviews of your work
- Hosting "devil's advocate" dinner debates
Post-Transformation Landmarks
Those who've navigated emotional barriers often report:
- Temporal Shift: Viewing conflicts through cosmic timeframes
- Sensory Enhancement: Finding profound beauty in mundane moments
- Quantum Compassion: Understanding antagonists as spiritual teachers
As Rumi's timeless wisdom reminds us: "Your task is not to seek love, but to remove all barriers within yourself that resist it." The ultimate liberation lies not in emotional avoidance, but in becoming so vibrantly alive that no external validation can amplify your inherent worth.